The IVF Process
Whether you’ve been trying to conceive for a while or are just beginning to explore your fertility options, in vitro fertilization (IVF) can be a hopeful and highly effective path to parenthood. Still, the idea of pursuing IVF, or any fertility treatment, can feel overwhelming. With so many steps, medical terms, and emotional decisions, it’s normal to feel uncertain or even a little scared.
At Kofinas Fertility Group, we understand that IVF isn’t just a clinical process but a deeply personal journey. That’s why we’re committed to providing a compassionate, patient-first experience in addition to cutting-edge fertility care. From your initial consultation through every step of IVF, our goal is to equip you with the knowledge and support you need to feel confident in your fertility journey.
This page walks you through the full IVF process and timeline, so you can move forward with clarity, knowing exactly what to expect and who you can count on for additional guidance.
”Excellent staff. Excellent doctors. Excellent care. These are the experts in infertility - the Kofinas group is well known nationally. They are very compassionate toward their patients and very thorough. Would recommend them in a heartbeat."
What Is IVF?
In vitro fertilization (IVF) is one of the most effective forms of assisted reproductive technology (ART). IVF helps individuals and couples achieve pregnancy by combining eggs and sperm outside the body in a lab setting. Once fertilized, the resulting embryo(s) are transferred into the uterus in hopes of successful implantation and pregnancy. IVF can be used with your own eggs and sperm, or with donor eggs, donor sperm, or a gestational carrier, depending on your specific situation.
Is IVF Right for Me?
While IVF represents an effective fertility treatment for many individuals and couples, it might not be the right solution for you. That’s why we begin with a comprehensive fertility assessment to first understand the cause of your infertility and then develop a tailored treatment plan based on your body and goals.
“Everything about my experience was wonderful, from the caring staff to the loving doctors who treated me like family. Everyone was very knowledgeable and sensitive to my experience. I have nothing but wonderful things to say about both my process and as well as the wonderful staff who helped me finally complete my family with two beautiful children.”

Evaluation and Preparation
Before beginning IVF, you and your partner will complete several key fertility tests to help personalize your treatment plan and understand the correct dosages of medications for your body.
These include:
- Ovarian reserve testing
- Semen analysis
- Uterine cavity evaluation
- Pap smear and mammogram (if applicable and not already up to date)
- STI screening
- Genetic carrier screening
- Practice embryo transfer (This helps understand the best technique for insertion. A real embryo is not used for this test.)

Pre-Stimulation Treatment
You will likely undergo a short course of pre-stimulation treatment before beginning the active phase of your IVF cycle. The goal of pre-stimulation treatment is to regulate your reproductive hormones and create the optimal environment for your ovaries to respond to fertility medications. While it may seem like a small step, it can significantly impact the effectiveness and predictability of the entire IVF cycle.
Typically, you’ll be prescribed a combination of estrogen and progesterone birth control pills or estrogen-only medication. The medication Lupron® (a GnRH agonist) will likely also be prescribed to prevent premature ovulation, and your plan may include Cetrotide® (a GnRH-antagonist) to prevent premature follicle development.
Benefits of Pre-Stimulation Treatment:
- Helps prevent the formation of ovarian cysts
- Regulates your menstrual cycle for consistent timing
- Suppresses natural hormonal fluctuations that could disrupt stimulation
- Synchronizes follicle development for more efficient egg retrieval
Baseline Evaluation
On day 2 or 3 of your menstrual cycle, you’ll come in for baseline bloodwork and ultrasound. If these tests confirm that your hormone levels and ovaries are in the right condition to start stimulation medications, you will then move on to the next step.

Ovulation Induction
Once your body is primed from pre-stimulation treatment, the next step is to encourage your ovaries to produce multiple mature eggs to maximize the chance of successful fertilization. Known as ovulation induction, this step marks the beginning of your active IVF cycle.
You will begin a carefully controlled regimen of fertility medications, usually self-injected into the stomach or thigh. These medications stimulate your ovaries to develop multiple follicles, each of which contains a viable egg. Stimulation usually lasts around 10 days, though timing varies from patient to patient.
Medications may include:
- Follicle-stimulating hormone (FSH) such as Gonal-F® or Follistim® to encourage follicle growth.
- GnRH antagonists (like Cetrotide® or Antagon®) to prevent premature ovulation and add protection from ovarian hyperstimulation syndrome.
The type and dosage of medication are tailored to your individual hormone levels, age, ovarian reserve, and how your body responds throughout the process.
Careful Monitoring and Personalized Adjustments
Throughout ovulation induction, we closely monitor your progress with:
- Blood Tests to track key hormone levels.
- Transvaginal Ultrasounds to measure follicle growth and development
This allows your care team to make real-time adjustments to your medication if needed. We are here every step of the way to provide support and answer questions as your cycle progresses. Contact us to learn more about how we personalize your IVF treatment plan.

Final Maturation and Trigger Injection
As your follicles mature, your care team will closely monitor their size and development through ultrasound and bloodwork. Once enough follicles have reached the optimal size, it’s time for the final step before egg retrieval.
You’ll be instructed to administer a “trigger shot”: a hormone injection that completes the final maturation of your eggs and prepares them for retrieval.
Egg retrieval is carefully scheduled for approximately 36 hours after the trigger shot. This timing is crucial to make sure your eggs are collected before ovulation occurs.
Your fertility specialist will give you detailed instructions on when and how to administer the injection, so everything proceeds on schedule. At this point, you're just one step away from retrieval day.
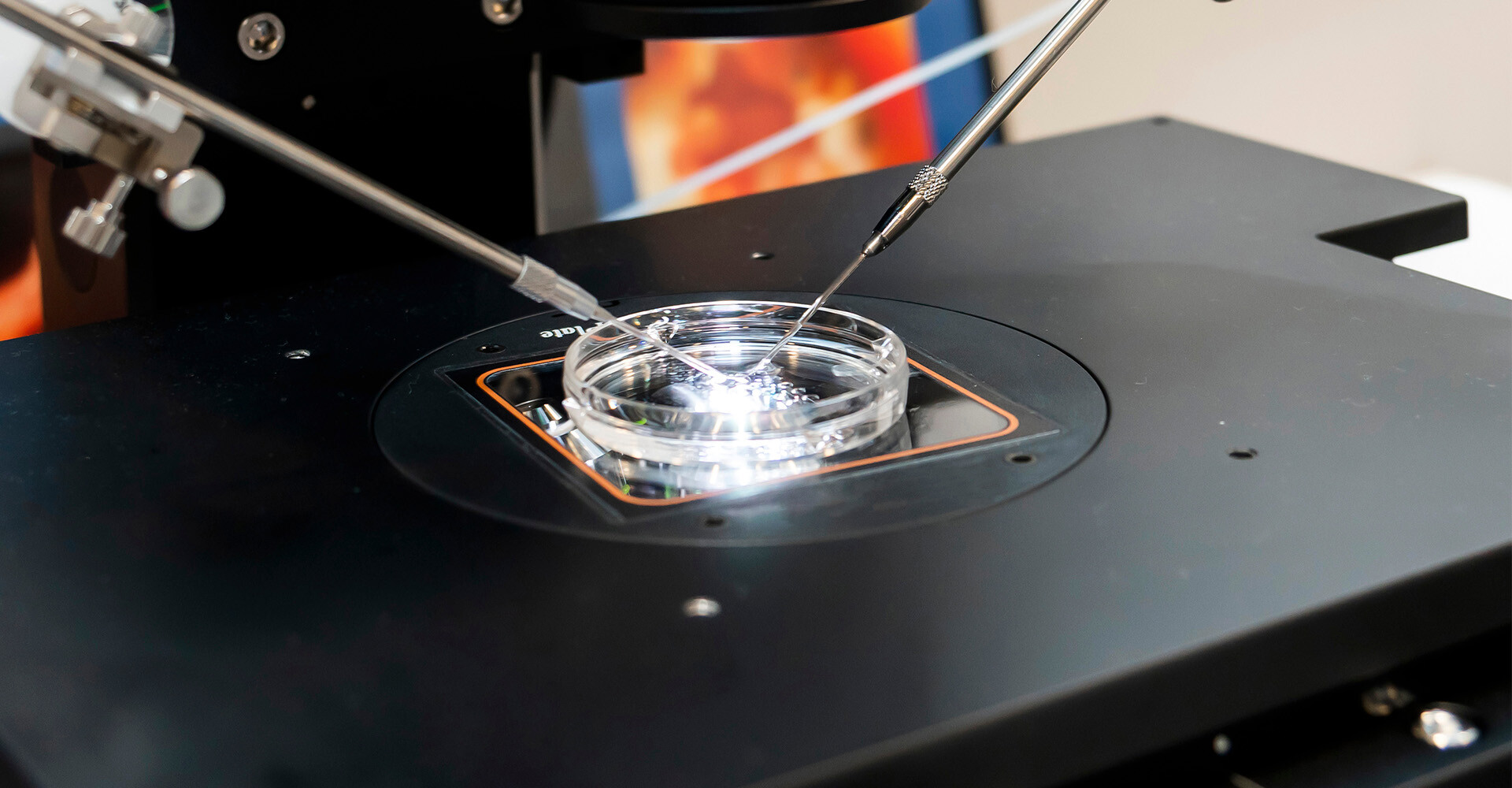
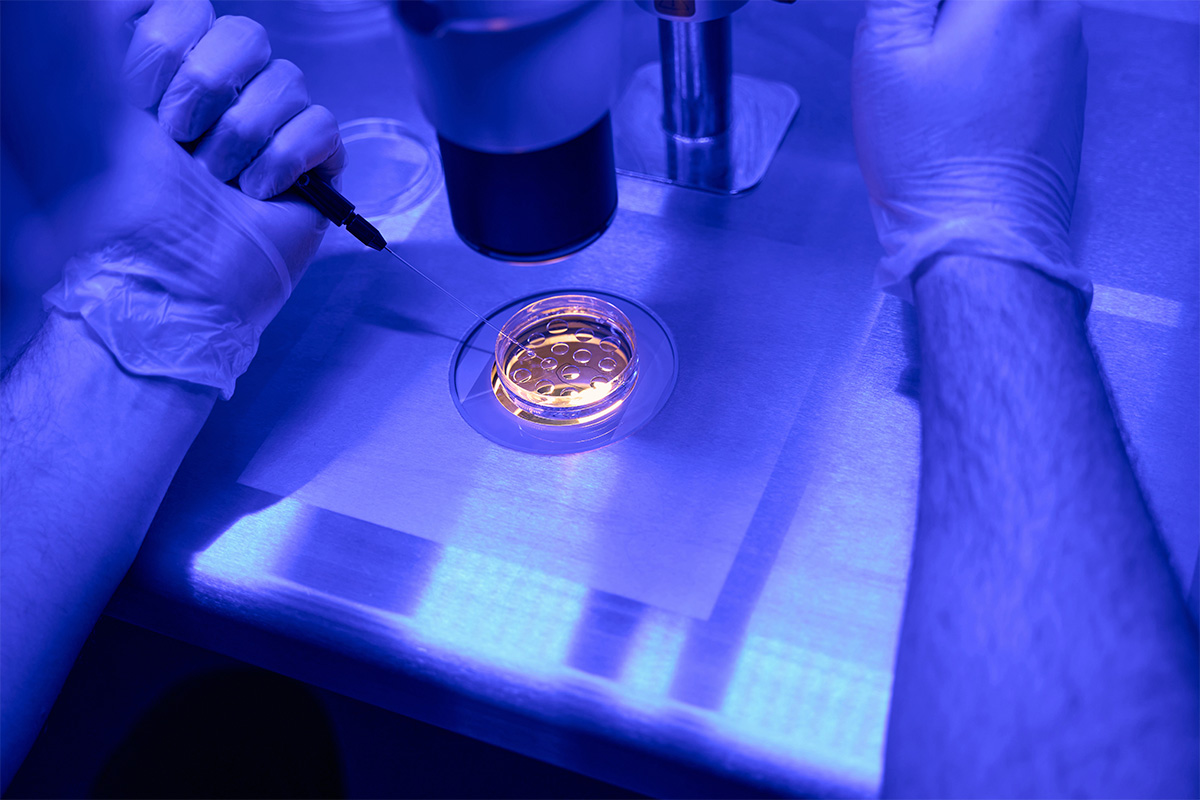
Egg Retrieval
Egg retrieval is a brief outpatient procedure that marks a major milestone in your IVF journey. This is when your mature eggs or your donor’s eggs are collected so they can be fertilized in the lab.
The procedure takes about 10-20 minutes and is performed under mild sedation to keep you comfortable. Using ultrasound guidance, your provider inserts a thin needle through the vaginal wall to gently aspirate eggs from the follicles on your ovaries. On average, 15 eggs are retrieved during the process.
After the Egg Retrieval Procedure
You’ll be monitored in recovery for a couple hours and discharged the same day, although you will need someone to drive you home after the procedure. Most patients are able to resume work and light activities within 24 hours, yet rest is still encouraged. Some mild cramping, bloating, or weight gain is normal and usually subsides within a few days.
While most women recover quickly, it’s important to stay in touch with your care team regarding your symptoms. Prior to egg retrieval, your fertility team will walk you through exactly what to expect before and after the procedure, so you know how to prepare.

Sperm Retrieval
A sperm sample is then collected to fertilize the retrieved eggs. This can be done in one of two ways:
- Fresh Sample: Sperm is provided via ejaculation at the clinic on the same day as egg retrieval. This is the most common way to obtain a sperm sample.
- Frozen Sample: In some cases, such as when a partner is unavailable or if you are used.
Your care team will work with you in advance to ensure the sperm retrieval method aligns with your treatment plan and timeline.

Fertilization
Once eggs and sperm are collected, the next step is to fertilize them in the lab. Fertilization is the method by which embryos are created and occurs the same day as your egg retrieval (or your egg donor's).
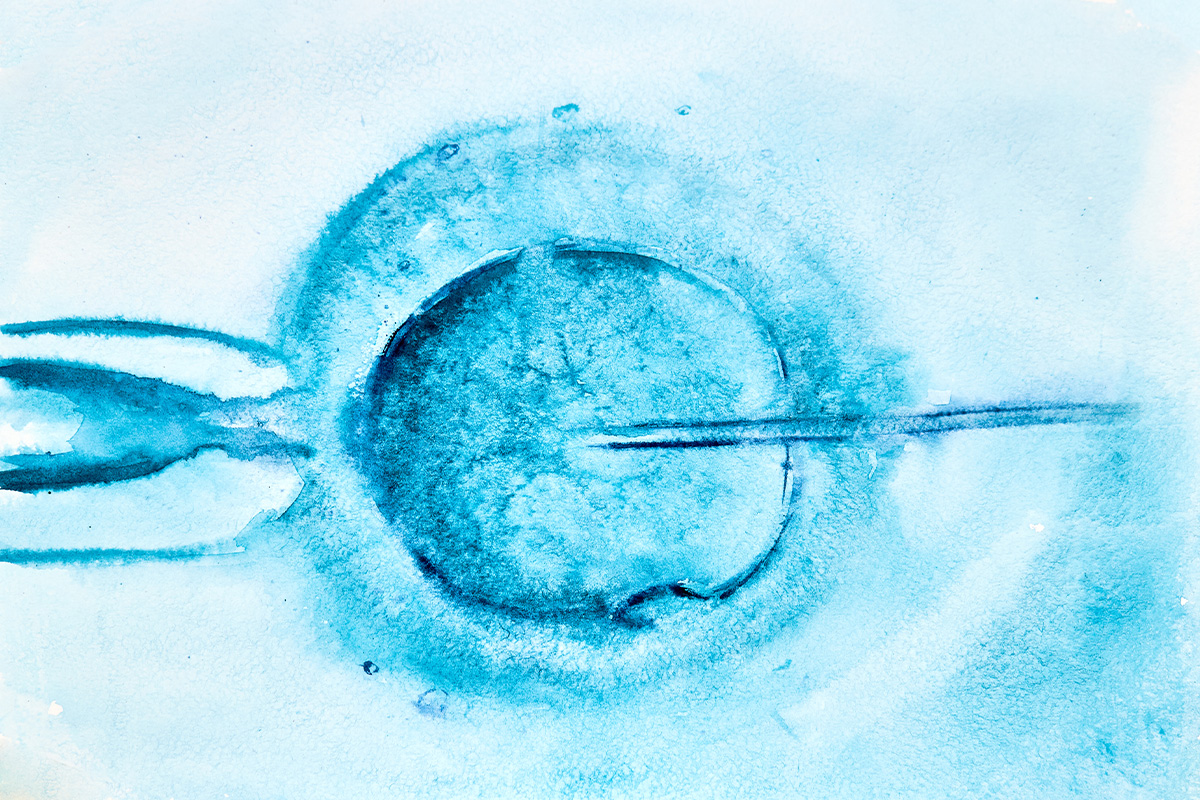
IVF Fertilization Methods
- Conventional Insemination: Healthy sperm and mature eggs are combined in a specialized incubator, allowing fertilization to occur naturally.
- Intracytoplasmic Sperm Injection (ICSI): In this more targeted method, a single sperm is injected directly into each mature egg. ICSI is often recommended for patients with male factor infertility or previous unsuccessful IVF cycles.
Understanding Success Rates
Your fertility team will carefully assess which method is most appropriate for your situation to give you the best chance of fertilization. IVF success rates depend on many factors, including age, fertility conditions, and the number of IVF cycles. We are privileged to support all hopeful parents on their journey and are proud of how many couples and individuals we’ve helped achieve their dreams.
“I recently underwent IVF fertility treatments at Kofinas Fertility, and I cannot express enough gratitude for the exceptional care provided by Dr. Jason Kofinas. His empathy, thoroughness, and unwavering commitment were instrumental in my successful journey. Thanks to Dr. Jason, I was able to bank embryos, get pregnant on my first transfer, and give birth to a perfectly healthy baby boy.”
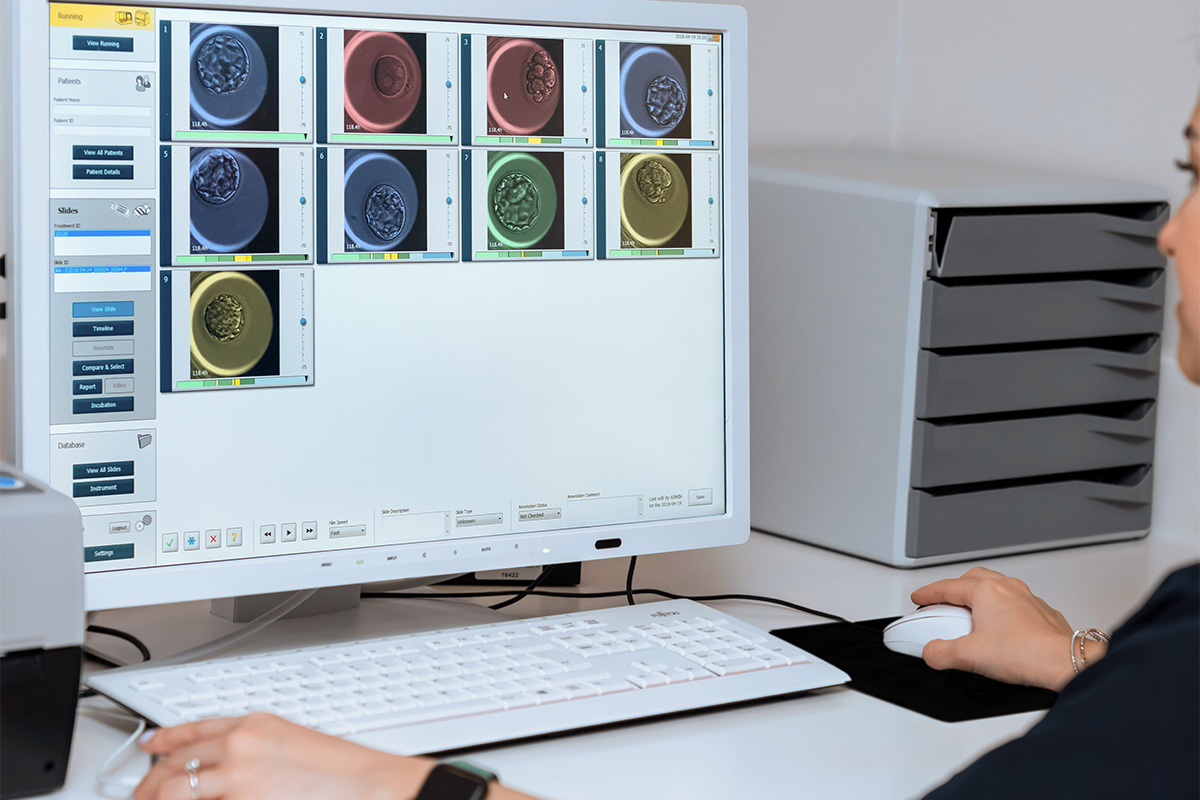
Embryo Monitoring
The day after fertilization, we receive a report detailing how many eggs successfully became embryos. These embryos are then closely monitored in the lab for several days to track their development and quality.
Watching for Blastocyst Development
Embryologists observe the embryos as they grow, which ideally reach the blastocyst stage by day 5 or 6. An average of 50% of embryos reach the blastocyst stage, indicating that they have developed to a point where they are ready for implantation or future freezing.
Each embryo is evaluated based on:
- Rate of cell division
- Cell symmetry and structure
- Overall developmental progress
These factors help determine which embryos are most viable for transfer or freezing. Fresh embryos will be transferred immediately, while frozen embryos can be saved for future use and implanted later.
Embryo Transfer
Embryo transfer is the moment you’ve been working toward. After fertilization, the fertilized embryo is transferred into your uterus (or your gestational carrier’s) to hopefully achieve pregnancy.
Fresh vs. Frozen Embryo Transfer
There are two primary approaches to embryo transfer:
- Fresh Embryo Transfer: Embryos are transferred a few days after fertilization, between days 3 to 5 of your cycle.
- Frozen Embryo Transfer (FET): Embryos are cryopreserved and transferred in a future cycle. FET offers greater flexibility in timing and is commonly used when donor eggs or previously frozen embryos are involved.
Thanks to advancements in cryopreservation, frozen embryo transfer success rates are comparable to fresh transfers, offering patients more options without compromising effectiveness.
The Embryo Transfer Procedure
The embryo transfer is a quick, 10-minute outpatient procedure. A thin catheter is gently guided through the cervix to place the embryo into the uterine cavity. No sedation is needed, and most patients describe it as similar to a pap smear. Between one and three embryos will be transferred, depending on factors such as age and embryo quality.
You’ll be asked to rest briefly before going home. It’s normal to experience mild cramping, spotting, or breast tenderness afterward.
If implantation is successful, the embryo will attach to the uterine lining within 6 to 10 days. During this waiting period, your care team will continue to support you with instructions and next steps.
If frozen embryos are used, the embryo transfer takes place at a later date. On day 21 of your cycle, you will complete an ultrasound and blood work, and then a round of hormones to optimize the success of the transfer.

Embryo Freezing
If you have multiple high-quality embryos following fertilization and monitoring, those not used during your initial transfer can be safely frozen (cryopreserved) for future use.
Embryo freezing offers the flexibility to expand your family on your own timeline, whether that’s months or years down the road. It also reduces the need for repeating ovarian stimulation and egg retrieval in future IVF cycles, making it a more efficient and less invasive option.
Kofinas Fertility Group can freeze and preserve your embryos for you. At this stage, we can also help you pursue preimplantation genetic testing (PGT) to assess the chromosomal quality of embryos. When you’re ready, frozen embryos can be carefully thawed and transferred.
When Should You Consider Embryo Freezing?
- Planning for a second child
- Delaying pregnancy due to health, personal, or career reasons
- Preserving fertility ahead of medical treatments (e.g., cancer therapy)
- Preparing for future FET (frozen embryo transfer) cycles
Request an appointment to learn more about embryo freezing and whether this step may be right for you.

Pregnancy Test
Two weeks after your embryo transfer, you’ll return to the clinic for a pregnancy blood test—the final step in the IVF process.
This test measures the level of human chorionic gonadotropin (hCG) in your blood, a hormone produced only if implantation has occurred. It’s more accurate than a home test and helps confirm whether the embryo has successfully implanted in the uterine lining.
What Happens Next
- If the test is positive, congratulations! Your journey continues with early pregnancy monitoring and continued use of certain medications through the first trimester to help maintain a healthy pregnancy.
- If the test is negative, your care team will meet with you to provide support, answer questions, and help you decide on next steps. This might include reviewing frozen embryos, adjusting your treatment plan, or taking a break before trying again.
No matter the outcome, you won’t face it alone. Our team at Kofinas Fertility Group brings a compassionate, patient-centered approach to your fertility journey. We are here to offer support, provide guidance, and help you move forward.
“The fertility process is a difficult one, so it’s so important to have doctors, nurses and staff at a facility that are caring, personable, friendly and invested in you as a person. You really need to be more than a cog to them. The whole team shares with you in the pain of loss and the joys of success. I cannot express enough how important it is to have that type of support.”
Kofinas Fertility Group brings over 70 years of combined expertise in reproductive medicine to help you achieve your dream of parenthood. Because we understand that every fertility journey is unique, we take a highly individualized approach to treatment, focusing on first identifying the root cause of your infertility.
From your first consultation through every stage of the IVF process, we prioritize transparency, clarity, and compassion. Our physicians, nurses, embryologists, and patient coordinators work together to provide seamless, coordinated support. Drawing on the latest advancements in fertility treatment, we combine innovation with heartfelt guidance to give you the best possible chance at success.
Request an Appointment
The IVF Process: FAQs
How long does the IVF process take from start to finish?
How many embryos are usually transferred in IVF?
What are the success rates of IVF?
Will I need more than one IVF cycle?
What can I do to prepare my body for IVF?
Can IVF help if I have a condition like PCOS, fibroids, or endometriosis?
Is IVF my only option?